Abstract
Introduction: CD34+ peripheral blood stem cells serve as the primary source for the majority of allogeneic stem cell transplants for hematologic malignancy, and adequate cell numbers must be infused to ensure engraftment. While the target dose is typically 5x106 cells/kg, there have been conflicting data on the effect of higher doses on outcomes. Due to concern for adverse effects, such as graft-versus-host disease (GVHD), some groups have suggested capping the CD34+ cell dose; however, various levels have been recommended, and the majority of studies have only small numbers of patients at very high cell doses where any effects may be most evident. In addition, manipulation of grafts can be time-consuming and lead to an increased risk of contamination. To better assess the effect of high cell dose on outcomes, we reviewed patients at our center who received matched unrelated donor (MUD) transplants with CD34+ dose in the highest quintile.
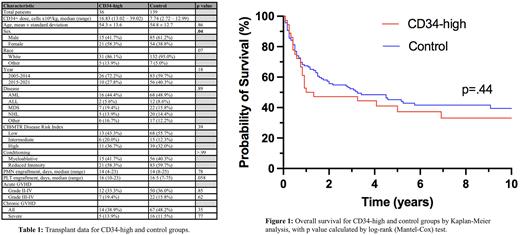
Methods: We performed a single-center retrospective analysis of adult patients with hematologic malignancy who received a MUD allogeneic stem cell transplant with CD34+ cell dose in the highest quintile (>13x106 cells/kg) from 2005 to 2021. Data were collected on patient and donor demographics, disease and transplant characteristics, and CIBMTR risk index. Outcomes were compared with the remaining MUD transplant patients during the same time period, including overall survival (OS), relapse-free survival (RFS), transplant-related mortality (TRM), GVHD rates and severity, and engraftment kinetics, with survival data censored at 10 years. Patients who received multiple transplants or had cryopreserved grafts were excluded. Neutrophil (PMN) engraftment was defined as the first of 3 consecutive days with absolute neutrophil count >500 cells/µL, and platelet (PLT) engraftment defined as the first of 3 consecutive days with PLT count >20x103 cells/µL and at least 7 days after most recent transfusion. Demographic data and GVHD rates were compared by Fisher's exact test or chi-squared test; age by Welch's t-test; engraftment kinetics medians by Mann-Whitney U test; and OS, RFS, and TRM by Kaplan-Meier analysis with log-rank (Mantel-Cox) test for significance.
Results: 36 patients were identified in the highest quintile with a median CD34+ dose of 16.83x106 cells/kg (range: 13.02-39.02) compared to 139 control patients with median dose of 7.74x106 cells/kg (2.72-12.99). Patients in the high-dose group were more likely to be female (58.3% vs 38.8%, p=.04), with no other statistically significant differences in donor, recipient, or disease characteristics (Table 1). There was a trend toward faster PLT engraftment in the CD34-high group (median 16 vs 16.5 days, p=.058), but there was no effect on PMN engraftment time (14 vs 14, p=.78). There was no difference in incidence of acute GVHD, either grade 2 or above (33.3% vs 36.0%, p=.85) or grade 3 or above (19.4% vs 15.8%, p=.62), and the groups showed similar incidence of chronic GVHD both overall (38.9% vs 48.2%, p=.35) and for severe disease (13.9% vs 11.5%, p=.77). There was no significant difference in OS between the two groups by Kaplan-Meier analysis (Figure 1, p=.44). Comparing the CD34-high group to the control group, the estimated 2-year survival was 47.2% vs 55.7%, and the estimated 5-year survival was 37.3% vs 45.2%. There was similarly no difference in RFS or TRM (p=.34 and p=.55, data not shown).
Conclusions: Previous studies of the effect of CD34+ cell dose on transplant outcomes have been limited by small numbers of patients at the highest doses. In this single-center study using one of the highest dose cutoffs in the literature (>13x106 cells/kg), we showed a trend toward faster PLT engraftment with no difference in GVHD incidence or mortality. As a retrospective study, a major limitation is possible confounding, and we plan to include other potential factors, such as GVHD prophylaxis, in multivariate analysis, though our initial results did not show major differences in baseline characteristics. In this cohort, patients receiving very high CD34+ cell doses had similar outcomes to those receiving standard doses. These data do not support the routine use of graft reduction by CD34+ cell number, which may help guide future practice.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal